Diseases
Knowledge is essential
Be aware of diseases that can affect a woman’s quality of life
- Cervical cancer
- Ovarian cancer
- Endometriosis
- Fibrome
- Adenomyosis
-
Polycystic ovarian
syndrome (PCOS) - Pregnancy loss
- Infertility
Cervical cancer
In the Democratic Republic of Congo (DRC), the incidence of cervical cancer is estimated at 30-35 per 100,000 population. In Kinshasa, the capital city, there are an estimated 3,500 new cases per year. Unfortunately, in this geographical location, incidence coincides with mortality (who).
Introduction
- More frequent in developing countries
- Second only to breast cancer (developed countries)
- Sexually transmitted disease (HPV) cellular transformation to invasive Kre can take an average of 13 years.
- Vaccination and screening are still the best way to prevent it because it is diagnosed at the pre-invasive stage
Risk factors
- Sexual activity (1st intercourse before 17 years and multiple partners), marriage before 20 years and multipartite more than ( Child before 20 years).
- Repeated genital infections
- Smoking
- Contraception
- Humanitarian deficiency
- Carcinogenic factor (role of circumcision)
Diagnostics
- Kre in situ has no clinical expression (screening by cervico-vaginal smear)
- Invasive Kre: metrorrhagia, leucorrhoea, pelvic pain.
- Confirmation: Anapath
Treatment and Evolution
- Prevention: early detection in all sexually active women and vaccination
- Curative or palliative: Depending on the stage but the principle is surgery, chemo, radiotherapy
- Evolution : Invasive Kre 2-10 years.
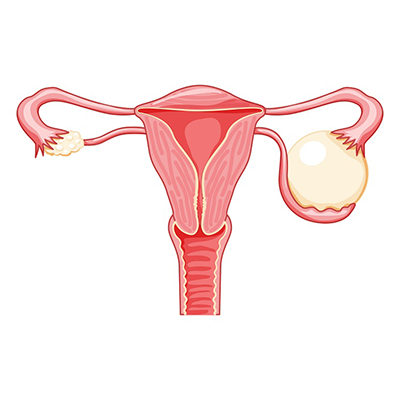
Ovarian cancer
Introduction
5th malignant tumor in the West after the breast, colon, cervix and body of the uterus, there are several benign tumors of the ovary that can become cancerous. The epidemiology is disappointing due to the difficulties of individualizing risk factors for screening.
Risk Factor
- Family factors 5% when a 1st degree relative is affected
- Nulluparity and sterility
- Ovulation-inducing treatment
Circumstances of discovery
- Clinical variable menstrual disorder (amenorrhe dysmenorrhee)
- Pelvic pain
- Adnexal mass
- Ascites
- NB: Always do histology after cystectomy
Treatment
- Surgery, chemo, radiotherapy depending on the stage
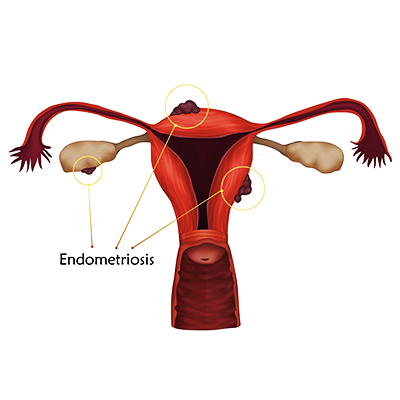
Endometriosis
Presence of morphologically and functionally endometrial tissue outside the uterine cavity:
A distinction is made between internal endometriosis or adenomyosis and external intra
peritoneal endometriosis
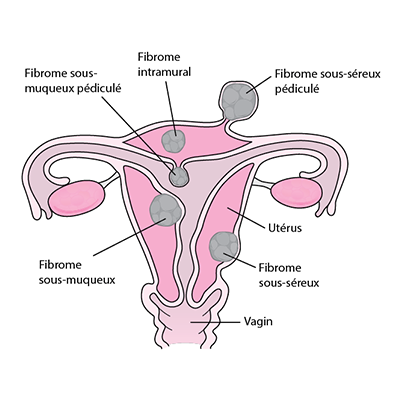
Fibrome
Synonym Uterine myoma, leiomyoma
DEFINITION AND CHARACTERISTICS: Benign tumor that develops at the expense of the muscle fibers of the uterus. Fibroids are the most frequent benign tumors in women; Europe: 20% of women from the age of 30 and 40% of women at the age of 50. This frequency increases in black women. The precise cause is not known: the fibroid would be the myometrial expression of a local hyperoestrogenism. Observations – Absence of myomas before puberty.
- Stabilization or regression of myomas after menopause or castration.
- Sudden increase during pregnancy and then regression.
- Increase sometimes after estroprogestive treatment.
Frequent association of endometrial hyperplasia (source of bleeding).
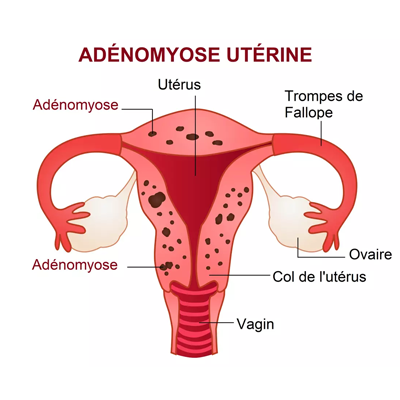
Adenomyosis
Penetration of endometrial diverticula into the thickness of the myometrium.
Favoring factors are:
- Trauma by pregnancy
- Uterine revision
- Curettage
- Experimental adenomyosis due to endometrial depression in the
scar and its surroundings
Causes
4 theories retained are :
- Transplantation of endometrial fragments due to menstrual reflux through the tubes, lymphatic or vascular metastases.
- Metaplasia by different stimuli which would lead to the development of endometrial tissue in a metaplastic position from the coelomic cells.
- Immunity by the acceptance and development of endometrial grafting from severe menstrual tubal reflux to an immune deficiency (autoimmune pathology).
- Genetics: presence of genes likely to favor the adhesion and development of the ectopic endometrium in progress.
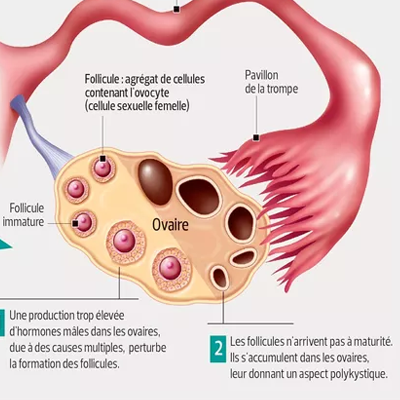
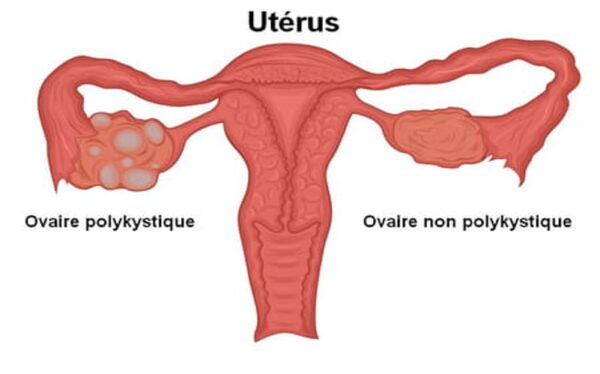
Polycystic ovary syndrome
Introduction
- Micropolycystic ovary syndrome is also called Stein-Leventhal syndrome. It is an endocrine (hormonal) disease that affects young women and is characterized by an increase in the level of male sex hormones (androgens) and an absence of ovulation (anovulation).
- The syndrome was first described by Irving F. Stein and Michael L. Leventhal in 1935;
- Micropolycystic ovary syndrome (MPOS) is the most common endocrine disorder, affecting 5% of women of reproductive age in France.
- It is the cause of more than 70% of infertility cases due to ovulation disorders.
- There is wide ethnic variation, with incidences well in excess of 10% in populations in Asia Minor, Central Asia, and the Indian Peninsula.
- Apart from the risk of infertility, PCOS is frequently associated with metabolic disorders.
- Patients have a later risk of high blood pressure, diabetes, with an increased risk of endometrial adenocarcinoma beyond menopause
- In the Democratic Republic of Congo (DRC), the incidence is not well known
- This chronic gynecological endocrine disease of unclear origin, but with probably a genetic and environmental component, mainly affects young women.
Favouring factors
- This pathology seems to be hormonal in origin since a deficit in luteinizing hormones and an excess of androgens, male hormones, are mostly found.
- Obesity (30-80%)
- Insulin resistance syndrome (Insulinoresistance)waist circumference greater than 88cm, blood sugar level ì
- Genetic abnormality (insulin receptor defect)
What are the symptoms
- Many symptoms are present in this syndrome which are expressed to different degrees depending on the woman.
- Among the most marked,
- Absence or disturbance of menstrual cycles (short and spaced periods
- Sterility (anovulation, consequence of the interruption of follicular maturation) Hirsutism (the excessive presence of hair on the chest, stomach and face) and acne.
- Android obesity (weight gain)
- Hair loss on the top of the head and signs of virilization are also possible but more rare
- Ultrasound: two large ovaries with several cysts
- Hormonal disorder (LH ⇑, FSH ⇓, Androgen testosterone⇑)
When to consult?
- If you have difficulty maintaining a normal weight, excess hair, acne, or irregular periods, consult a doctor
Illustration
Treatment
- MHD( lifestyle adjustment) A healthy lifestyle and balanced diet combined with daily physical activity (exercise for weight loss) is the most important part of treatment.
- A drug treatment can be prescribed to regulate the menstrual cycle, and to reduce the growth of hair and acne.
- If pregnancy is desired: ovulation inducer and/or surgery
References
- J Lansac,C Paillat: grand livre de gynecologie,2019
- Journal of General Medicine and Continuing Medical Education 2021) www.who.int
- https://www.univadis.es ‘ viewarticle ‘ endo–2022–who…
- https://pro.endocrineweb.com ‘ conference–news ‘ insu…
- https://www.stylist.co.uk ‘ fitness-health ‘ wellbeing
- https://pcoschallenge.org ‘ pcos–news
- infertility guidelines 2022
- polycystic ovarian syndrome guidelines
Pregnancy loss
There are two types: spontaneous and induced. In this module we will discuss spontaneous abortions, which, by definition, are when the fetus dies. Approximately 20-30% of women who have a confirmed pregnancy have a hemorrhage during the first 20 weeks of pregnancy; half of these women have spontaneous abortions. Thus, the incidence of spontaneous miscarriage is up to about 20% of confirmed pregnancies. The incidence for all pregnancies is probably higher, as some very early abortions are mistaken for delayed menstruation. Fetal death or expulsion of products of conception have several denominations depending on the term:
ranges up to about 20% of confirmed pregnancies. The incidence for all pregnancies is probably higher, as some very early abortions are mistaken for delayed menstruation.
Fetal death or expulsion of products of conception has several names depending on the term :
- Spontaneous abortion: fetal death, sometimes with removal of products of conception (fetus and placenta), before 20 weeks gestation
- Late fetal death: death of the fetus a ≥ 20 weeks
- Preterm delivery: expulsion of a live fetus between 20 and 36 weeks/6 days Abortions can be classified as follows (see table Classification of abortions):
- Early or late
- Recurrent (also called repeat abortion)
- Septic
Approximately 10-15% of confirmed pregnancies abort spontaneously. Up to 25% of all pregnancies end in spontaneous abortion during the first 12 weeks of pregnancy. The incidence for all pregnancies is probably higher, as some very early abortions are mistaken for delayed menstruation.
Causes
Une fausse couche spontanée précoce est souvent provoquée par des anomalies chromosomiques. Les anomalies maternelles (p. ex., utérus bicorne, fibromes, adhérences) peuvent également entraîner une perte de grossesse avant les 20 semaines de grossesse. Les fausses couches spontanées isolées peuvent être dues à certains virus, les plus notables étant le cytomégalovirus, l’herpès virus, le parvovirus et le virus de la rubéole. D’autres causes comprennent des anomalies immunologiques et un traumatisme majeur. Le plus souvent, la cause reste inconnue. Les facteurs de risque de fausse couche spontanée comprennent :
- Age > 35 years
- History of spontaneous miscarriage
- Smoking
- Use of certain drugs (e.g., cocaine, alcohol)
- A poorly controlled chronic condition (e.g., diabetes, hypertension, overt thyroid disorder) in the mother
Subclinical thyroid disorders, uterine retroversion, and minor trauma have not been shown to cause spontaneous miscarriage.
Infertility
We speak of the sterility of the couple when after 18 months to 24 months, 2 people of different sex, having regular sexual relations without any notion of contraception, there is no pregnancy.
Anglo-Saxon schools currently speak of 12 months.
- Fertility: The probability that a couple will conceive during a cycle.
- Infertility: Inability to conceive
- Fertility: Ability to carry a pregnancy to term
- Infertility: Conception occurs but the pregnancy is not carried to term.
NB: For the Anglo-Saxons, sterility and infertility say the same thing. Primary sterility: if there has never been fertilization Secondary sterility: if the woman, after one or more pregnancies and whatever the outcome (miscarriage, EP), is not fertilized even though she wants to be.
In order for fertilization to occur, certain factors are taken into account:
- Female factors, Age – Quality of ovulation -, Quality of cervical mucus, Quality of fallopian tubes, Fertility of the oocyte, Receptivity of the endometrium,…
- Male factors – Concentration, mobility and morphology of spermatozoa – Lack of fertility.
- Factors related to the couple – Frequency of sexual intercourse